Most people think of hospital safety in terms of hand sanitizer, training, and technology. And while all of those matter, there's one factor that often flies under the radar: the actual building itself. Yep, the walls, hallways, layout, and even lighting of a hospital can either support great care or set the stage for costly mistakes.
It might sound surprising, but poor design has a ripple effect. When a nurse can’t find the right room fast enough or a surgeon has to deal with glare in the operating room, patient outcomes can suffer. And when they do, families sometimes turn to a medical negligence lawyer to figure out what went wrong—and if it could’ve been prevented.
Let’s take a closer look at how hospital architecture quietly shapes patient safety—and what some facilities are doing differently to reduce risk before it even begins.
Design Isn’t Just About Aesthetics—It’s a Safety Tool
When we talk about design, it's easy to think about fancy lobbies or cozy recovery suites. But hospital architecture is more than a facelift for patient satisfaction surveys. Thoughtful design can directly impact how efficiently care is delivered—and how often mistakes are avoided.
Take room layout, for instance. If a patient’s room is designed so that the bed faces away from the entrance, a nurse might not see them struggling or calling for help. If supply rooms are too far from patient areas, staff might delay care while running around for materials. Small delays or missed cues like these can turn into major problems.
Simple tweaks—like ensuring line of sight between nurses’ stations and patient beds or placing sinks in prominent locations to encourage hand washing—can make a real difference.
The Role of Lighting and Acoustics in Error Prevention
Lighting in hospitals isn't just about brightness. It’s about clarity and comfort. Poor lighting can cause fatigue, particularly for staff working long shifts. It can also increase the chances of misreading charts, medication labels, or even patients’ facial expressions.
Daylight, on the other hand, has been shown to boost mood and alertness—not just for patients, but for the healthcare workers tending to them. Natural light in areas like nurses’ stations and patient rooms has been linked to fewer errors and better job satisfaction.
Sound also plays a surprisingly big role. Constant beeping, alarms, and overlapping conversations create cognitive overload, making it harder for medical staff to focus. Some newer hospitals are now integrating acoustic panels and smart layouts to reduce noise levels without compromising awareness. It’s a balance—but one worth finding.
How Layout Affects Communication (and Mistakes)
Here’s a scene that plays out in hospitals more often than we’d like: A medication change is handed off from one shift to the next, but the message gets lost—or misinterpreted. Boom. A preventable mistake.
The way a hospital is laid out affects how easily staff can communicate, whether casually or in structured handovers. Units designed with long, sprawling hallways or isolated corners can reduce face-to-face interaction, which increases the chance that critical info falls through the cracks.
More open, decentralized layouts—where nurses work in smaller pods closer to patient rooms—can encourage communication and collaboration. These designs allow for faster response times and more personal attention, which naturally lowers the risk of oversights.
Infection Control Starts With the Floorplan
When it comes to preventing infections, cleaning protocols and hand hygiene are just the beginning. Design plays a critical role in infection control too.
Some hospitals have shifted to single-patient rooms not just for comfort, but to reduce cross-contamination. Shared rooms are riskier—especially during flu season or in the age of airborne viruses.
Additionally, the placement of hand-washing stations, trash disposal areas, and even airflow direction (yep, air moves in planned ways!) can all either help or hinder infection prevention efforts. A well-designed HVAC system with proper zoning can help limit the spread of pathogens from one part of the hospital to another.
Tech Integration: The Built Environment Has to Keep Up
As hospitals adopt more digital tools—from bedside barcode scanners to voice-activated charting systems—the physical environment has to keep up. That means enough outlets, proper Wi-Fi coverage, and even wall mounts for devices that reduce clutter and tripping hazards.
It also means designing spaces where monitors and mobile carts can move freely, without blocking access to emergency exits or bumping into beds. Thoughtful design here isn’t about tech for tech’s sake—it’s about making sure innovation actually supports safer care.
Staff Wellbeing = Patient Safety
Here’s something that’s becoming clearer every year: Tired, stressed, and burned-out staff make more mistakes. So hospital design that supports staff wellbeing isn't a luxury—it's a safety investment.
This includes break rooms with natural light and quiet zones. It includes dedicated walking paths for quick decompression. Some forward-thinking hospitals have even added green spaces or access to nature within the facility.
When staff are mentally and physically supported by the space they work in, they’re sharper, faster, and more emotionally present with patients. That’s a win for everyone involved.
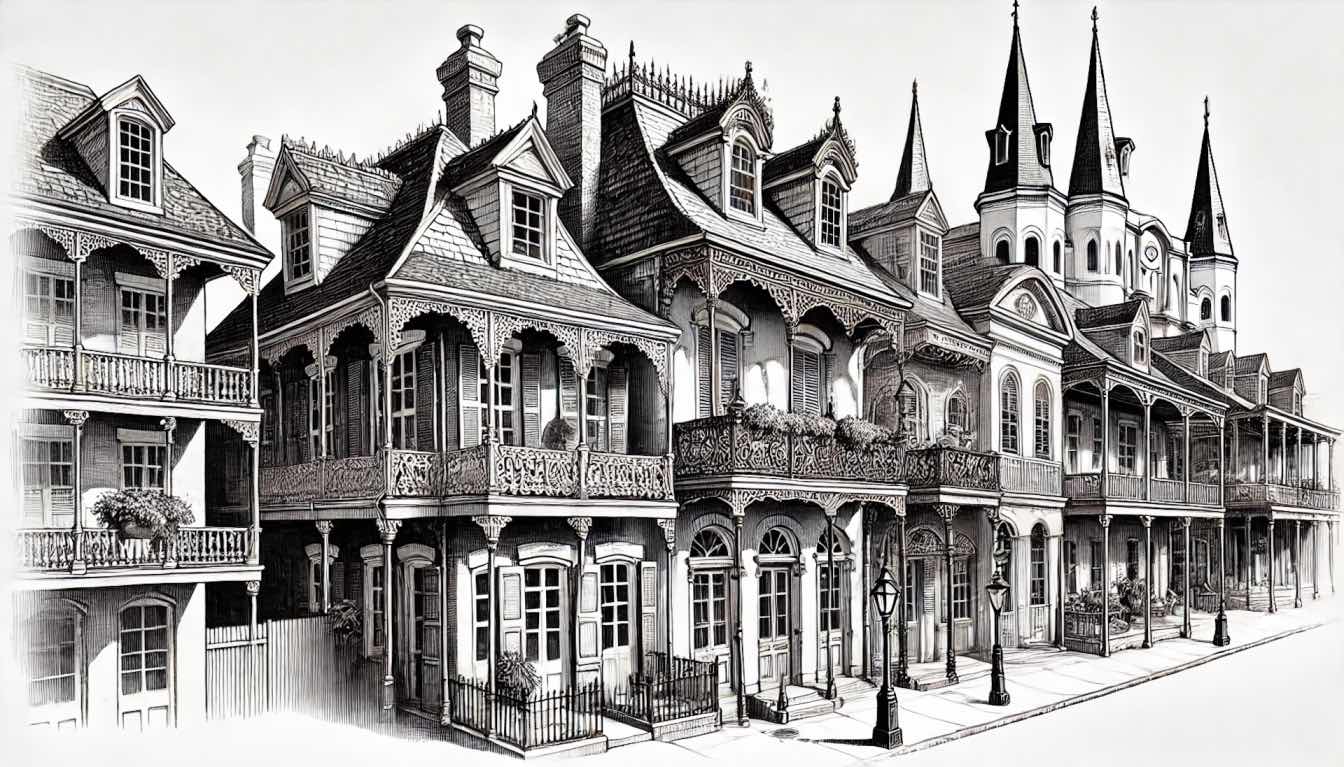
Real-World Examples of Design Changes That Work
Plenty of hospitals have already made changes after seeing how design impacts safety. Here are a few examples:
Virginia Mason Medical Center in Seattle redesigned their operating rooms to streamline equipment access. The result? Fewer surgical delays and a significant drop in setup-related errors.
The Cleveland Clinic shifted to same-handed patient rooms, meaning every room is laid out exactly the same. That way, staff don't need to reorient themselves every time they walk in—critical seconds are saved, and consistency reduces mental load.
Singapore’s Khoo Teck Puat Hospital uses abundant natural light, garden views, and airflow optimization throughout its facility—creating a space that’s not only beautiful but also clinically effective.
Why This Conversation Matters Now
Healthcare environments are changing fast. There’s more pressure than ever to provide safe, efficient care while also controlling costs. So hospitals have to do more than react—they need to design for safety from the ground up.
That’s especially important in aging facilities that were built for different times and different needs. As patient expectations shift and staff burnout becomes a larger concern, the need for design-forward thinking only grows.
It’s no longer enough to have good policies. Hospitals need good spaces too.
What Patients (and Families) Should Keep in Mind
You don’t have to be an architect to understand how a hospital’s design can impact care. If you’re visiting or choosing a facility, here are a few things to casually look out for:
1. Are patient rooms single or shared?
2. Is it easy to spot hand-washing stations?
3. Do the nurses seem close by and visible?
4. Does the space feel chaotic or calm?
These cues can offer clues into how much thought has been put into the environment—and how well that space is set up to avoid errors.
If something ever does go wrong, understanding the role of design may also help when talking to care teams or seeking advice from a medical negligence lawyer. Sometimes, the problem isn’t just what happened—but how the setting made it more likely.
Final Thoughts: The Quiet Power of Smart Design
Hospital design isn’t just about aesthetics or efficiency—it’s about safety. Every layout choice, lighting decision, or hallway width carries ripple effects that can shape a patient’s experience and outcome.
The best-designed hospitals work behind the scenes. They make it easier for staff to do their jobs. They keep patients safer without anyone even realizing why. And most importantly, they prevent problems before they start—not just fix them after the fact.
When hospitals are built smarter, everyone wins.